What is BFR (Blood Flow Restriction) Training?
The ACL Road to Recovery - Blood Flow Restriction
The ULTIMATE BFR Tutorial (Blood Flow Restriction)
Blood Flow Restriction | Science, How To & 3 Wins Over Traditional Training – (26 Studies)
How To Stop Walking Hunched Over! 5 Best Fixes
The heart has to work very hard if you have aortic stenosis, a condition where the aortic valve narrows and blood cannot flow normally.
Our life literally hangs on how well blood is pumped through our four heart chambers with the help of four heart valves (aortic, mitral, pulmonary and tricuspid), which open and close with each heartbeat.
Imagine the precision and intricacies of a healthy heart – it beats 100,000 times a day during which the mitral and tricuspid valves control blood flow between the heart chambers.
The pulmonary valve controls blood flow to the lungs while the aortic valve controls blood as it flows out from the heart’s lower left chamber to the aorta, the main artery bringing blood to the rest of the body.
A life-threatening condition
Your heart will then need to work harder to pump blood to the rest of your body, affecting your health and limiting your daily activities.
This condition is called aortic stenosis and it’s a progressive disease that ranges from mild to severe.
Often, this condition may go unnoticed as patients go about their daily lives discounting the irregularities in their well-being.
Aortic stenosis is the most common valvular heart disease worldwide, with its prevalence increasing with age.
It is estimated that up to 12.4 % of people over age 75 have aortic stenosis, and about 80% of adults with symptomatic aortic stenosis are male.
Symptoms generally occur when narrowing of the aortic valve is severe.
However, some people with aortic stenosis may not even have symptoms for many years.
If you demonstrate symptoms such as chest pains or discomfort during physical activity, dizziness, fatigue, shortness of breath and an irregular heartbeat, don’t dismiss it.
Consult a physician.
Understanding the disease
If diagnosed with aortic stenosis, it means your aortic valve is not opening or closing properly.
This limits the amount of blood pumped out to your body and strains your heart.
Over time, the left ventricle of your heart can thicken and enlarge.
Heart muscles will weaken and this can lead to heart failure and complications such as stroke, blood clots, bleeding, irregular heart rhythms and infections of the heart.
Left untreated, it can be fatal. It is important to understand the difference between aortic stenosis, atrial fibrillation and myocardial infarction.
While all are cardiovascular related, they are different and require different treatment approaches.
Atrial fibrillation is a disorder that originates from the atrium (upper chambers of the heart).
When the atrium does not contract effectively, irregular and rapid heart rhythm occurs.
Blood can pool in the heart, running the risk of blood clots which may lead to stroke.
Myocardial infarction, commonly known as a heart attack, occurs when there is a rupture of an atherosclerotic plaque in a coronary artery.
This causes a blood clot that obstructs blood flow.
Very simply put, aortic stenosis is a valve disorder, atrial fibrillation is an irregular heart rhythm and myocardial infarction is a heart attack caused by a blocked coronary artery.
Root cause
Some individuals may be born with aortic valve disorders and are more prone to aortic stenosis later in life.
Other causes include infection of the heart, chronic kidney disease, heart disease risk factors such as diabetes, high cholesterol and high blood pressure, or a result of radiation therapy.
Diagnosis and evaluation
If aortic stenosis is suspected, your cardiologist will recommend diagnostic tests, as outlined below, depending on the assessment of your condition.
> An ultrasound imaging test called an echocardiogram to visualise the aortic valve and assess its structure and condition.
This test identifies weakened muscles and determines the severity of the aortic stenosis.
> An electrocardiogram or ECG measures the electrical activity of the heart and detects any potential issues with the heart’s chambers.
> A chest x-ray determines the condition of the heart and lungs and detects if there is swelling in
the aorta and/or calcium build-up on the aortic valve.
> If needed, a cardiac computerised tomography (CT) scan or a cardiac magnetic resonance imaging (MRI) may be done.
> Only when needed or when other non-invasive test are inconclusive, a cardiac catheterisation or a cardiac angiogram may be recommended.
Treatment modalities
Lifestyle modifications are necessary, regardless of the stage of your aortic stenosis.
Start consuming a hearthealthy diet.
Eat a variety of fruits and vegetables, low-fat or fat-free dairy products, poultry, fish and whole grains.
Avoid saturated and trans-fat and excessive salt and sugar.
If you are overweight, lose weight through regular exercise; brisk walks each day are recommended.
Manage your stress levels. Indulge in wholesome activities.
If you are a smoker, consider quitting.
In cases of mild aortic stenosis, your cardiologist will prescribe medications which are a non-invasive.
It can provide a temporary relief of symptoms and may reduce risk of complications.
However, medications alone do not address the underlying valve issues.
Patients may risk a decline in their condition over time.
Thus, it is essential to diligently keep your regular heart checkups to monitor the progression of your condition.
In more severe cases, aortic stenosis patients may have to undergo procedures to repair or replace their defective valves such as :
> Balloon valvuloplasty (BAV)
> Surgical aortic valve replacement (SAVR)
This offers a longer lifespan for the replaced valve and is often the conventional treatment for aortic stenosis.
However, being an open-heart surgery, it carries inherent risks especially for elderly patients and those with underlying health conditions.
These surgical valve replacements may also wear out over time and can start to fail and causes stenosis and regurgitation (valve does not fully close and blood flows backward through the valve).
Patients are advised to stay in the hospital for seven days.
> Transcatheter Aortic Replacement (TAVR)
This is a minimally invasive procedure performed between one to two hours as compared to an invasive open-heart surgery.
A small cut is made in the groin, neck or between your ribs so that a thin, flexible tube with the TAVR can be guided and placed in your diseased valve.
The new valve will then work immediately, and the tube is removed.
TAVR is designed to work like your own heart valve as the materials used allow the frame to mold itself to your anatomy.
It’s worth noting that the artificial TAVR valve can be made of porcine or bovine materials.
This procedure is suitable for patients who are considered highrisk or unsuited for open-heart surgery.
Patients can consult their cardiologist for other suitability criteria.
This involves shorter hospital stays of about three days as patients recover faster.
Institut Jantung Negara (IJN) was the first hospital in Malaysia to do a TAVR procedure in 2009.
At that time, some in the medical fraternity shared their uncertainty about the durability or longevity of a TAVR and thought it may only last for five years or less.
They preferred conventional surgery which was known to last for about 10 years.
The TAVR has since grown in acceptance and has been proven to stand the test of time.
For 83-year-old aortic stenosis patient, Siti Rahmah, who was implanted with a TAVR in 2011, it has still been functioning effectively.
She recently shared, “I am very pleased with the progress I have made. It has been 12 years since I did the procedure. I am thankful that I can go about my daily activities quite comfortably. My condition has been well managed.”
Take action
Those at-risk patients and 65 years and above should never undermine the importance of regular heart check-ups to detect irregularities of the heart.
Aortic stenosis is a serious cardiovascular condition.
Left untreated, it can lead to significant health problem while early diagnosis and a personalised treatment can prolong life.
By Datuk Dr Shaiful Azmi Yahaya is a senior consultant cardiologist at Institut Jantung Negara. For further information, email starhealth@thestar.com.my. The information provided is for educational and communication purposes only, and it should not be construed as personal medical advice. Neither The Star nor the author gives any warranty on accuracy, completeness, functionality, usefulness or other assurances as to such information. The Star and the author disclaim all responsibility for any losses, damage to property or personal injury suffered directly or indirectly from reliance on such information.
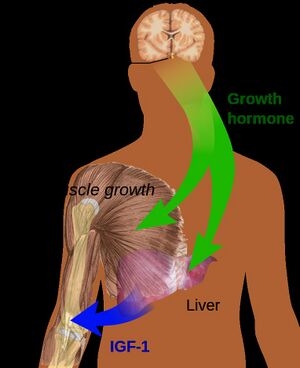
Any exercise, resistance or aerobic, brings about a significant increase in human growth hormone (HGH). Insulin-like growth factor and growth hormone are responsible for increased collagen synthesis after exercise and aids muscle recovery. Growth hormone itself does not directly cause muscle hypertrophy but it aids muscle recovery and thereby potentially facilitates the muscle strengthening process.[15] The accumulation of lactate and hydrogen ions (eg in hypoxic training) further increases the release of growth hormone. [13]
High intensity training has been shown to down regulate myostatin and thereby provide an environment for muscle hypertrophy to occur.[12] Myostatin controls and inhibits cell growth in muscle tissue. It needs to be essentially shut down for muscle hypertrophy to occur.



